
Understanding ECLIPSE Claiming
Getting paid by Medicare, DVA & Health Funds has never been so simple. Through Services Australia Medicare Online & ECLIPSE claiming channels, there is less paperwork, shorter payment turn around times and funds are deposited directly in your bank account within days.
If you are a specialist provider or hospital organisation, we’re sure that you are aware of ECLIPSE. You may not be aware of all the benefits. In this article we’ll set out in black and white exactly what ECLIPSE is, what it can do, how you use it and how long the claim process takes. Finally, we share how you can implemented ECLIPSE claiming into your practice.
Where better to start than going back to basics.
What Is ECLIPSE Claiming?
ECLIPSE claiming allows specialist providers and hospitals to send in-patient medical claims (IMC) to participating health funds. This is done electronically via a secure internet connection.
Services Australia (previously known as Medicare Australia) provides and maintains ECLIPSE.
Transmissions are encrypted for maximum security and privacy of information.
ECLIPSE is only available through Practice Management Software which has undergone rigorous integration testing.
Services Australia does not charge for transmissions via ECLIPSE, yet you will need to pay for the software to transmit claims.
With ECLIPSE, you are only able to send claims that are up to 2 years old from the current date.
ECLIPSE Features Explained
As you can see on the Services Australia website, there are a number of different features.
The following list if the main features available as part of the ECLIPSE claiming:
- OPV PVM – Online Patient Verification Patient Verification Medicare;
- OPV PVF – Online Patient Verification Patient Verification Fund;
- OEC ECM – Enterprise Patient Verification Patient Verification Medicare;
- OEC ECF – Enterprise Patient Verification Patient Verification Fund;
- IMC – In-Patient Medical Claims; and
- ERA – ECLIPSE Remittance Advice.
The Service Australia web page above does not go into any depth on any of these features.
Below is a brief explanation of each.
FYI – there are also extended features of ECLIPSE claiming that might interest your healthcare organisation. You can find a quick explanation of what these are in this article.
OPV PVM – Online Patient Verification Patient Verification Medicare
This feature allows a practice to check the Medicare card information you entered for a patient into your practice management software, against the information held by Medicare Australia. A response is returned within seconds.
You will be asked the date of service prior to sending the Medicare card for verification.
If all the Medicare Card information is correct, an eligible code will be returned.
If there are any issues with the information sent, the Department of Human Services will return a code that will indicate the issue with the Medicare Card information you requested validation for. You can then update the Medicare Card information held for the patient and repeat the verification check.
A verification check can be performed an unlimited amount of time for your patients.
This reduces the risk of a claim being rejected because of outdated information.
OPV PVF – Online Patient Verification Patient Verification Fund
Much like the Medicare feature, this feature allows practices to check the Health Fund information that you entered for a patient against what is held against their Health Fund. This also checks that a patient had a valid policy on the date that you provided the service. A response is returned within seconds.
You will be asked the date of service prior to sending to the Health Fund for verification.
If all the Health Fund information is correct, an eligible code will be returned.
If there are any issues with the information sent, the Health Fund will return a code that will indicate the issue with the information. You can then update the information held for the patient and resubmit a verification check.
A verification check can be performed an unlimited amount of time for your patients.
This reduces the risk of a claim being rejected because of outdated information or the patient not having a valid policy at the time you performed the service.
OEC ECM – Enterprise Patient Verification Patient Verification Medicare
This feature differs from patient verification in that it is going a step further than checking to see if the patient’s information is the same as Medicare.
OEC relates directly to Online Eligibility Checking. This allows practices to check what Medicare benefit will be payable for the in-patient medical services provided and hospital stay for a patient.
To perform this check, you will need to know the provider, anticipated admission date and location for the in-patient services to be provided.
This report can then be used to provide a basis for the patient’s informed financial consent.
These reports are not real time and can take up to 20 minutes to be provided. These reports are then available for 7 days from the time it is made available.
OEC ECF – Enterprise Patient Verification Patient Verification Fund
Like the feature above, this also relates to Online Eligibility Checking. But this is a check against the patient’s health fund.
This verification allows practices to obtain an estimate of out of pocket expenses for the patient for the expected in-patient medical services and hospital stay.
To perform, you will need to know the provider, anticipated admission date and location for the in-patient services to be rendered.
This report can then be used to provide a basis for the patient’s informed financial consent.
These reports are not real time and can take up to 20 minutes to be provided. These reports are then available for 7 days from the time it is made available.
IMC – In-patient Medical Claim
An in-patient medical claim is when a provider sends a claim for services rendered to an admitted patient to Medicare and a Health fund.
Approved practice management software can send these in-patient medical claims electronically via ECLIPSE.
Every software solution does this differently but with the same end result.
ERA – Eclipse Remittance Advice
The Eclipse Remittance Advice (ERA) outlines the payment made for a lodged in-patient medical claim. Your practice management software picks up this report and allocates it against your claim.
In short – it tells you what you have been paid for the IMC claim.
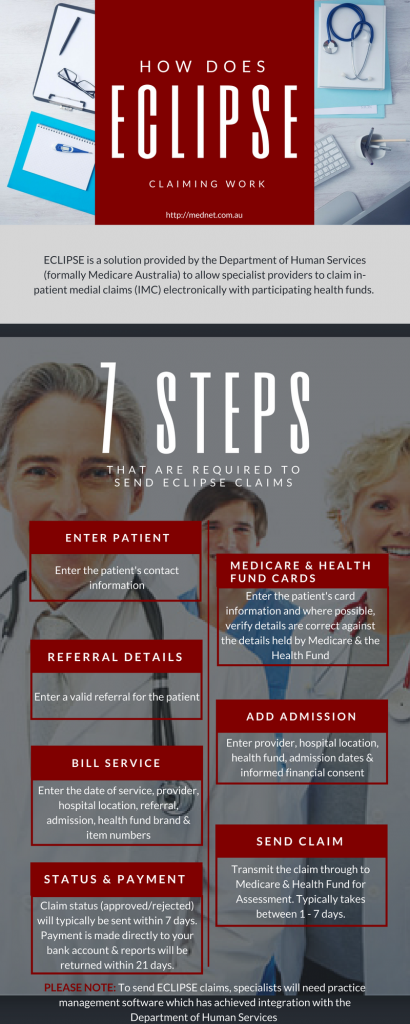
How Does ECLIPSE Claiming Work?
Software vendors handle the how of ECLIPSE claiming completely differently. Yet the sequence of processes needed remains the same across the board.
In a nutshell the sequence for ECLIPSE claiming is:
Timeline of an ECLIPSE Claim
Compared to sending claims manually in paper form to health funds, ECLIPSE drastically reduces the turnaround time from submission to payment to reporting. This will significantly improve your cash flow.
After you have completed your billing data entry, you will need to connect the Department of Human Services and send your claim. The Department of Human services will confirm they received your submitted claim (via an acknowledgement to your practice management software). This becomes the submission date. The Department of Human Services forwards the claim through to the health fund.
The Health Fund will respond to the Department of Human Services within 7 days of your submission date to advise if the claim is being paid and how much is being paid.
Rejected claims will be notified at this stage. This will also include a reason, allowing you to rectify and resubmit with a shorter turnaround time.
Department of Human Services returns this message as a processing report to your practice management software. You will see the dollar amount to expect or the reason for the rejection.
The health fund will issue an ECLIPSE remittance advice no later than 21 days of your submission date. The health fund will also deposit the funds into your nominated bank account.
The timing varies from health fund to health fund, so it is impossible to give definite dates you will physically receive your funds. Manual claims, on the other hand, can take in excess of 4 weeks.
What Health Funds Participate in ECLIPSE?
Just about all health funds participate in receiving claims through ECLIPSE.
Services Australia keeps information up to date on their website. You can view all participating health funds at: https://www.servicesaustralia.gov.au/private-health-insurers-functions-and-contact-details
What Do You Need To Do To Setup ECLIPSE
ECLIPSE claiming is only available through practice management software that has integrated the functionality through testing with the Services Australia.
MedNet’s practice management software is accredited for ECLIPSE claiming.
Want to find out how MedNet can get you claiming quickly?
Our team are specialists for online claiming, and especially ECLIPSE.
Contact us today to discuss your specific needs, and how we can help you setup quickly to get paid faster.
Call us on 1300 765 110 or fill out the form below.
MedNet Group Pty Ltd
Level 1, Unit 4
4 – 6 Kingsway
Cronulla, NSW, 2230
Email: info@mednet.com.au
Phone: 1300 765 110 (intl +61 2 9556 1498)